What is Inflammation and how Mitochondria combat Chronic Inflammation
“Our understanding of biology would be incomplete
without learning how it is associated with inflammation.”
– Ruslan Medzhitov, PhD, Sterling Professor of Immunobiology, Yale University
In this article, we explain what inflammation is, what problems cause inflammation, typical signs of inflammation, the difference between acute and systemic chronic inflammation, the relationship between chronic inflammation, macrophages and mitochondria and how mitochondria can trigger or combat inflammation.
Five Cardinal Signs of Inflammation
- Loss of function – swelling, for example, of a joint, may physically prevent movement and movement of an inflamed area can result in pain
- Swelling – fluid accumulation in extravascular areas (outside lymph vessels and blood vessels) due to increased membrane permeability
- Pain – activation of inflammatory mediators like Bradykinin and Histamine which stimulate nerve endings causing pain
- Heat – due to vasodilation and increased blood flow
- Redness – due to vasodilation and increased blood flow
Four Problems that cause Inflammation
Now that we’ve established the signs of inflammation, let’s explore the four types of problems which can cause inflammation:
- Loss of structure
- Loss of function
- Loss of regulation
- Loss of recognition
The loss of structure (for example, tissue injury) has traditionally been the most researched type of issue associated with inflammation. We now know that the first three types of problems that cause inflammation are interconnected in that structure provides function and function enables regulation.
When there is a loss of structure or tissue injury due to physical trauma, it causes loss of function – like when a twisted ankle causes weakness and loss of movement in the joint and loss of homeostasis or regulation in the affected tissues. When there is loss of regulation due to dehydration or starvation, the body struggles to maintain homeostasis and there is a loss of structure and function of cells and tissues.
Loss of structure, function and regulation in turn trigger an inflammatory response in the body.
The fourth cause of inflammation involves a biological loss of self-recognition. The body immune system is activated and attacks itself thinking that a particular molecule does not belong to a given system (for example, the brain, heart, thyroid, joints, etc).
Acute vs. Systemic Chronic Inflammation
While acute Inflammation is important for surviving and recovering from physical injuries and infections, environment, lifestyle and social changes in our lives today is creating Systemic Chronic Inflammation (SCI) that is the leading cause of many diseases.
Several causes of low-grade SCI and their consequences have been established. The most prevalent causes of SCI include aging, poor diet, physical inactivity, (visceral) obesity, poor gut health or intestinal dysbiosis, psychological stress, social isolation, fragmented sleep and disrupted circadian rhythm, and exposure to xenobiotics like air pollutants, hazardous waste products, industrial chemicals and tobacco smoking.
The most common consequences of SCI include osteoarthritis, metabolic syndrome (high blood pressure, high blood sugar, excess body fat around the waist, and abnormal cholesterol or triglyceride levels), type 2 diabetes, cardiovascular disease, non-alcoholic fatty liver disease (NAFLD), osteoporosis (loss of bone), sarcopenia (loss of muscle), depression, neurodegenerative diseases, auto-immune diseases and cancer.
equivalent to 74% of all deaths globally.”4
– World Health Organization
Risk Factors for Chronic Inflammation
- Aging – Cells, tissues, and organs are, as any other biological systems, are prone to the “wear and tear” that comes with time. The contribution of inflammation to aging-associated diseases is such that the term inflammaging is commonly used. A perfect example is the development of osteoarthritis as we age.
- Behavioral Risk Factors – It’s likely no surprise that the use of alcohol and tobacco, and the lack of exercise and an unhealthy diet significantly increase the occurrence of NCDs.
- Metabolic Risk Factors – Hypertension (high blood pressure), hyperglycemia (high blood glucose levels), hyperlipidemia (high fat levels in the blood) and obesity.
- Environmental Risk Factors – The term exposome is used for environmental exposure (internal, external, chemical, physical, biological, and social) that a person has during their lifetime and how these factors affect their biology and health. Several environmental risk factors trigger NCDs but the majority of the harm stems from air pollution and can manifest in strokes, ischemic heart disease, chronic obstructive pulmonary disease, and lung cancer.
Mitochondria play a crucial role in Macrophage biology
Growing evidence suggests that mitochondria in cells are involved in the interplay between metabolism and innate immune responses. Mitochondria act as scaffolds for many proteins where they help bind and organize protein molecules that are involved in immune signaling pathways that modulate the function of these proteins. They are also responsible for releasing a variety of molecules, such as ROS ( reactive oxygen species), which can modulate the immune response.
- ROS Production: reactive oxygen species (ROS) are stimulated during mitochondrial respiration. Macrophages use ROS to destroy pathogens during phagocytosis.
- Calcium Regulation: mitochondria regulate intracellular calcium levels. Macrophages require exact calcium signaling for immune responses.
- Apoptosis: Mitochondria are instrumental in apoptosis (programmed cell death). Macrophages can experience apoptosis to reduce inflammation or remove infected cells.
Healthy mitochondria provide energy, influence macrophage activation, and participate in a variety of cellular processes critical for immune function. The opposite is true as unhealthy mitochondria can either promote or simply impair immune function. Thus, it is critical to maintain healthy mitochondrial status.
- Energy Production: mitochondria are the powerhouses of the cell, generating ATP (adenosine triphosphate) through oxidative phosphorylation. Macrophages require ATP for different cellular processes, including phagocytosis (engulfing pathogens) and cytokine (signaling protein) production.
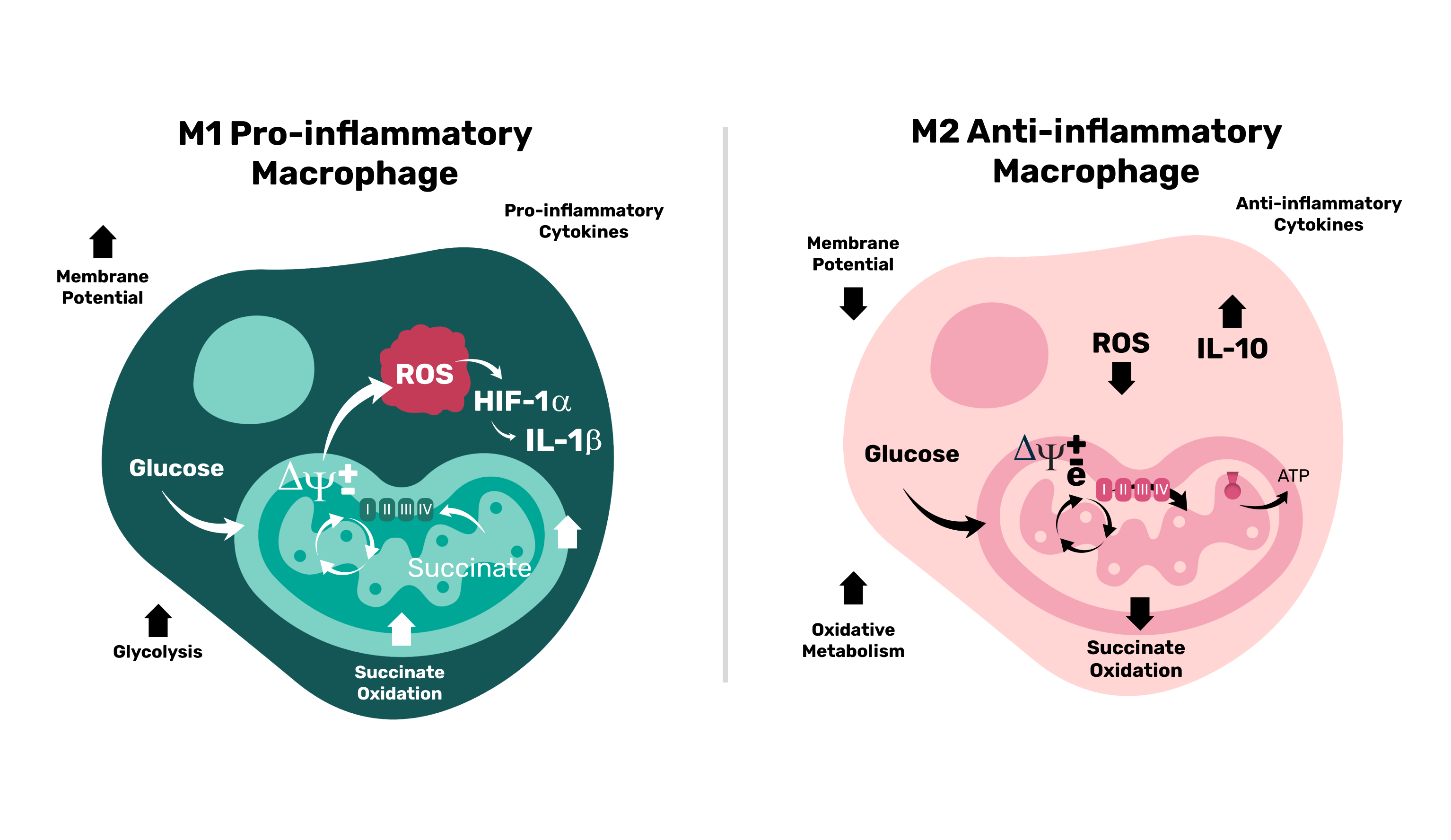
- Metabolism: macrophages alternate between M1 and M2 activation states based on their environment. This switch is directly influenced by mitochondrial metabolism. For example:
- M1 macrophages (pro-inflammatory) are glycolysis-dependent (where energy is produced in the cytoplasm of cells).
- M2 macrophages (anti-inflammatory) use oxidative phosphorylation (where energy is produced inside the mitochondria in the cell).
- ROS Production: reactive oxygen species (ROS) are stimulated during mitochondrial respiration. Macrophages use ROS to destroy pathogens during phagocytosis.
- Calcium Regulation: mitochondria regulate intracellular calcium levels. Macrophages require exact calcium signaling for immune responses.
- Apoptosis: Mitochondria are instrumental in apoptosis (programmed cell death). Macrophages can experience apoptosis to reduce inflammation or remove infected cells.
Boost mitochondrial health to combat Chronic Inflammation
- Eating a healthy diet rich in antioxidants
- Engaging in regular exercise and strength training
- Trying intermittent fasting
- Practicing breathwork exercises
- Getting the appropriate exposure to sunlight
- Reducing exposure to toxins and chemicals
- Undergoing heavy metal detoxification
- Reducing physical and mental stress
Read Next
- Salugenesis – Body’s innate healing process
- Impact of lifestyle & aging mitochondria on longevity and wellness
References
- Backman,I. (2021, Dec. 20). Inflammation Is a Fundamental Part of Physiology: New Approaches by Yale Immunobiologist. Yale School of Medicine. https://medicine.yale.edu/news-article/inflammation-is-a-fundamental-part-of-physiology-new-approaches-by-yale-immunobiologist/
- Medzhitov, R. (2021).The spectrum of inflammatory responses. Science, 374(6571), 1070-1075. https://www.science.org/doi/10.1126/science.abi5200
- Furman, D., Campisi, J., Verdin, E., et al.(2019). Chronic inflammation in the etiology of disease across the lifespan. Nat. Med, 12, 1822-1831. https://www.ncbi.nlm.nih.gov/pmc/articles/PMC7147972/
- Who Health Organization. (2023, September 16). Noncommunicable Diseases. World Health Organization. https://www.who.int/news-room/fact-sheets/detail/noncommunicable-diseases
- Mills, E., Kelly, B., Logan, A. et al. (2016). Succinate Dehydrogenase Supports Metabolic Repurposing of Mitochondria to Drive Inflammatory Macrophages. 50 Cell, 167(2), 457-470.https://www.cell.com/cell/fulltext/S0092-8674(16)31162-X
- Know, L. (2019). Mitochondria and the Future of Medicine: The Key to Understanding Disease, Chronic Illness, Aging, and Life Itself. Chelsea Green Publishing.
- Lam, M.(2024). An In Depth Look At The Bioenergetics Circuit: Pancreas, Liver, and Thyroid. Dr. Lam Coaching, https://www.drlamcoaching.com/articles/the-crucial-role-of-the-bioenergetics-circuit/



